It is very important to keep your blood sugar under control as uncontrolled diabetes (both type 1 and 2) can cause severe long term complications and can be life threatening.
long term complications of uncontrolled diabetes:
- Cardiovascular disease: The risk of stroke, heart attack and coronary artery disease arises due to damage in large blood vessels (atherosclerosis). The blood vessels gets narrowed due to:
- Damage to the artery wall
- Fatty streaks (cholesterol gathers around the artery wall and forms fatty streak)
- formation of plaque (the fatty streak becomes thick and hard in nature)
- Artery narrowing (The more build up of plaque the more artery walls thickens which leads to the reduction of blood flow)
- Plaque Rupture & Clot Formation (Sometimes the surface of a plaque can rapture leading to the body's clotting system to repair it which forms a blood clot. This clot narrows or can completely block the artery.
- Kidney Damage (Diabetic Nephropathy): High blood sugar damages kidneys filtering function which can lead to chronic kidney disease and even kidney failure.
- Nerve Damage (Diabetic Neuropathy): Affects legs and feet. It can cause:
- Tingling sensation
- Numbness
- Pain
- Loss of feeling
- Eye Damage (Diabetic Retinopathy): Uncontrolled diabetes can damage small blood vessels in the retina that cause vision problems and can ultimately lead to blindness in adults. It also increases the risk of glaucoma.
- Skin diseases: Can increase the risk of bacterial and fungal infection.
- Gum problems: Uncontrolled diabetes can lead to gum inflammation or periodontitis, an advanced gum disease.
These long term or chronic issues develop over time and damage the blood vessels and nerves throughout the body.
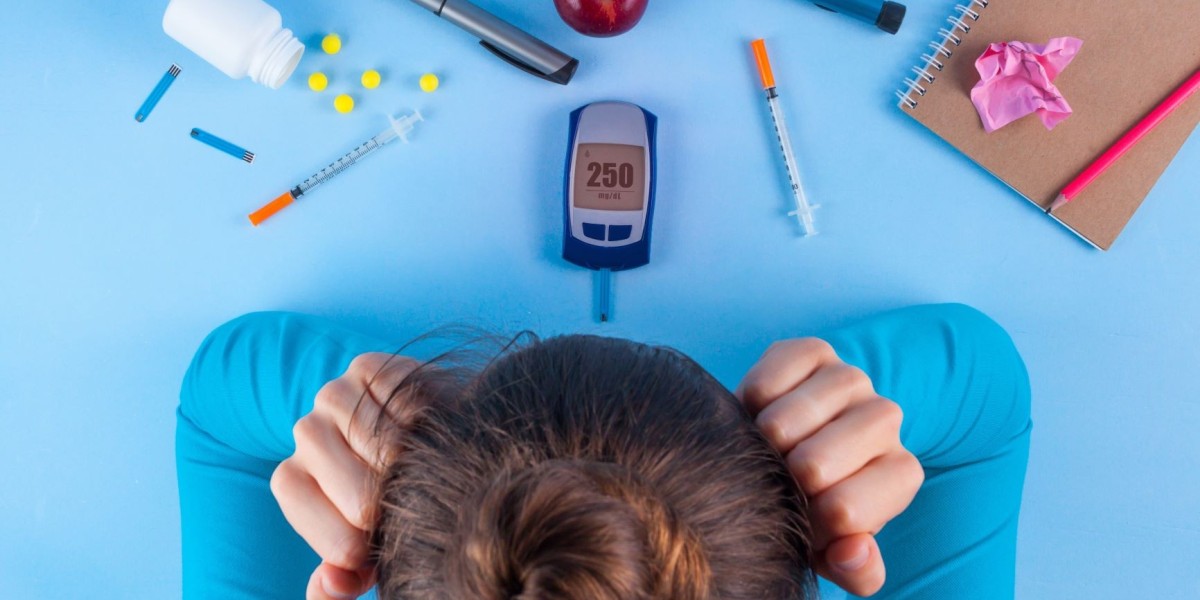
So, what should you do if you have uncontrolled diabetes?
The action plan requires a combination of medical intervention, rigorous monitoring, and committed lifestyle changes.
Immediate medical and monitoring steps:
Work closely with your Doctor or healthcare provider to stabilize your condition.
Consult Your Doctor:
Schedule an urgent appointment with your primary care doctor and/or endocrinologist. They will review your current medication regimen (or start one if you aren't taking any).
Intensify Monitoring:
You must check your blood sugar more frequently, sometimes up to 4 to 8 times a day (before and after meals, at bedtime, and overnight), to see how food, stress, and medication are affecting your glucose levels. Discuss getting a blood glucose monitor or a CGM device, which gives real-time glucose readings and shows trends, making it much easier to catch and prevent highs and lows.
Medication Adjustment:
Your doctor will likely adjust your oral diabetes medications or insulin therapy (type and dosage) to aggressively target your A1c goal.
Screen for Complications:
Since your diabetes has been uncontrolled, your doctor will order specific screenings such as
- HbA1c: To measure your average blood sugar over the past 2–3 months.
- Lipid Panel: To check cholesterol and triglycerides (crucial for cardiovascular risk).
- Kidney Function: Blood and urine tests (like the albumin-to-creatinine ratio) to check for early diabetic nephropathy.
- Dilated Eye Exam: See an ophthalmologist (not just an optometrist) for a comprehensive check for diabetic retinopathy.
- Foot Exam: Check for early signs of diabetic neuropathy and poor circulation.
Essential Lifestyle Adjustments
Lifestyle changes are the foundation of controlling blood sugar and improving insulin sensitivity.
Optimized Nutrition (Diet)-
- Carbohydrate Management: This is the single biggest factor in blood sugar control. Work with a Certified Diabetes Care and Education Specialist (CDCES) or Registered Dietitian to learn:
- Carb Counting: Accurately calculating the carbohydrate grams in your meals to match your insulin/medication dose.
- Focus on Fiber: Prioritize high-fiber, complex carbohydrates (whole grains, beans, non-starchy vegetables) which slow sugar absorption.
- Eliminate Sugary Drinks: Strictly cut out all sodas, sweet teas, juices, and sweetened coffees, as these cause the fastest, highest blood sugar spikes.
- Portion Control: Use the Plate Method (half non-starchy vegetables, one-quarter lean protein, one-quarter whole grain/starchy vegetable) to manage intake.
Physical Activity-
- Improve Insulin Sensitivity: Exercise makes your muscles more sensitive to insulin, allowing them to absorb glucose from the bloodstream more effectively.
- Consistency is Key: Aim for at least 150 minutes of moderate-intensity aerobic exercise per week (e.g., brisk walking, swimming) and incorporate strength training 2-3 times per week.
- Post-Meal Movement: A 10–15 minute walk after a meal can significantly lower the resulting blood sugar spike.
Manage Weight and Stress-
- Weight Loss: Losing even 5–10% of body weight can dramatically improve blood sugar, blood pressure, and cholesterol levels.
- Stress Reduction: Chronic stress releases hormones (like cortisol) that raise blood sugar. Incorporate stress management techniques like deep breathing, meditation, or spending time outdoors.
- Prioritize Sleep: Poor sleep increases insulin resistance. Aim for 7–9 hours of quality, uninterrupted sleep per night.
Crucial Self-Care and Preventative Measures
These steps directly address the long-term complications you listed.
- Foot Care:
- Inspect your feet daily for cuts, blisters, redness, or swelling.
- Wear comfortable, well-fitting shoes and moisture-wicking socks.
- Never walk barefoot.
- Blood Pressure and Cholesterol: Uncontrolled diabetes and high blood pressure/cholesterol are a triple threat to your heart and arteries (Cardiovascular Disease and Atherosclerosis). Take any prescribed medications for these conditions exactly as directed.
- Quit Smoking: Smoking severely restricts blood flow and accelerates every single long-term diabetes complication (especially nerve damage and kidney disease). Quitting smoking is mandatory.
For more information, visit: onlinegenericmedicine.com