According to FutureWise analysis, the healthcare fraud analytics market in 2025 is US$3.48 billion, and is expected to reach US$17.02 billion by 2033 at a CAGR of 21.95%.
The healthcare fraud analytics market is experiencing significant growth due to rising financial losses from healthcare fraud, waste, and abuse, which cost the global system billions each year. This concerning trend highlights the urgent need for advanced detection mechanisms to address these issues effectively. Enter the game-changers: artificial intelligence (AI) and machine learning algorithms. These technologies are revolutionizing fraud detection by revealing complex patterns and anomalies in claims data that traditional systems often overlook. As governments implement stricter regulations and oversight, particularly in public insurance programs, healthcare payers and providers are compelled to invest heavily in sophisticated fraud analytics platforms.
Additionally, the rapid transition to digital health records and the rise of telemedicine have introduced new vulnerabilities, creating new opportunities for fraudulent activities. This shift has increased the demand for real-time monitoring solutions capable of detecting billing irregularities, identity theft, and phantom billing schemes across various channels. The need for innovative strategies in fraud detection has never been more critical to protecting our healthcare systems.
FutureWise Market Research has published a report that provides an in-depth analysis of Healthcare Fraud Analytics Market trends that will affect overall market growth.
Request a Free Sample @
https://www.futurewiseresearch.com/contact.aspx?rpt=5797&type=requestsample
By Solution Type
- Descriptive Analytics
- Predictive Analytics
- Prescriptive Analytics
By Application
- Insurance Claims Review
- Postpayment Review
- Prepayment Review
- Pharmacy Billing Misuse
- Payment Integrity
- Other Applications
By Delivery
- On-Premise Delivery Models
- On-Demand Delivery Models
By End User
- Public and Government Agencies
- Private Insurance Payers
- Third-Party Service Providers
- Employers
By Region
- North America
- Europe
- Asia-Pacific
- Latin America
- Middle East and Africa
Competitive Landscape in Healthcare Fraud Analytics Market:
- IBM
- Optum (A Part of Unitedhealth Group)
- Cotiviti Holdings, Inc.
- Fair Isaac Corporation
- SAS Institute
- Change Healthcare
- EXL Service Holdings, Inc.
- Wipro
- Conduent, Inc.
- HCL Technologies
- CGI Group
- DXC Technology Company
- Northrop Grumman Corporation
- LexisNexis (A Part of Relx Group)
- Pondera Solutions
Buy now the latest version of this report: https://www.futurewiseresearch.com/checkout.aspx?ReportId=5797&license=multi
**Objectives of this Study: **
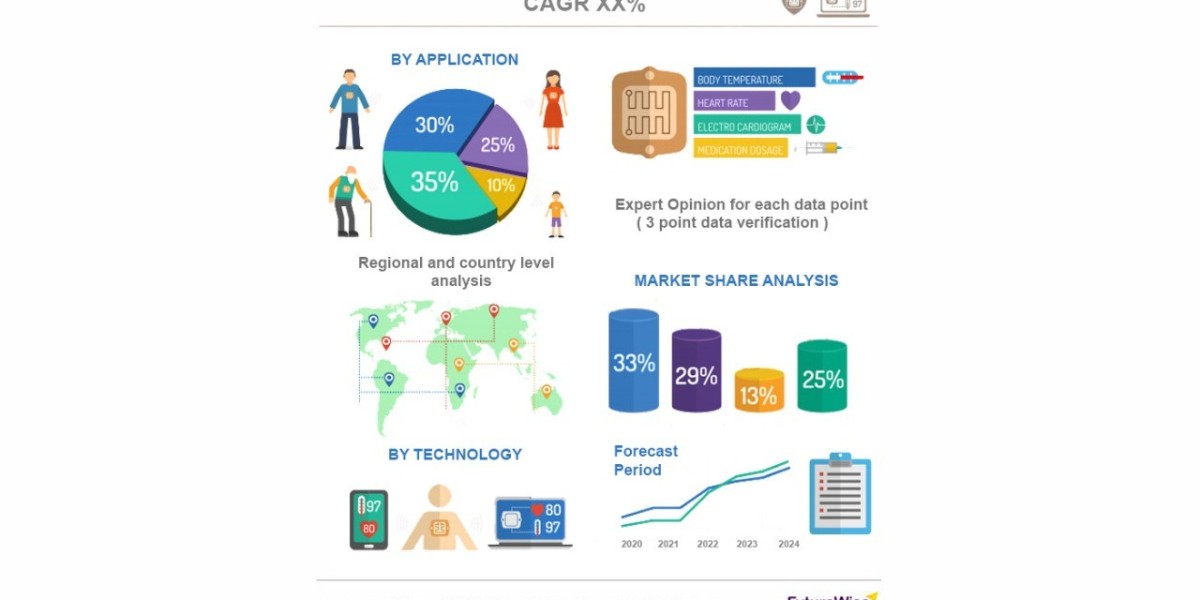
- To provide a comprehensive analysis of the Healthcare Fraud Analytics Market By Solution Type, By Application, By Delivery, By End User and By Region.
- To offer detailed insights into factors such as drivers, restraints, trends, and opportunities, as well as segmental and regional influences on market growth.
- To evaluate current market trends and forecast micro-markets, presenting overall market projections in the form of data sets and PowerPoint presentations.
- To predict the market size in key regions, including North America, Europe, Asia Pacific, Latin America, and the Middle East and Africa.
Flexible Delivery Model:
- We have a flexible delivery model and you can suggest changes in the scope/table of contents as per your requirement
- The customization services offered are free of charge with the purchase of any license of the report.
- You can directly share your requirements/changes to the current table of contents to: [email protected]