History and Discovery of Induced Pluripotent Stem Cells
The groundbreaking discovery of induced pluripotent stem (iPS) cells in 2006 marked a major turning point in the field of regenerative medicine. A team of Japanese scientists led by Shinya Yamanaka was the first to demonstrate that adult mouse cells could be reprogrammed to an embryonic stem cell-like state through the insertion of four transcription factors. Just two years later, human iPS cells were derived using the same approach. This seminal finding meant that patients' own cells could potentially be transformed into any cell type in the body, circumventing ethical issues surrounding the use of embryonic stem cells. Since the original studies, iPS cell technology has advanced rapidly, aided by improvements in reprogramming methods and the development of integration-free iPS cell lines. Today, iPS cells hold immense promise for modeling diseases, drug discovery, and personalized regenerative therapies.
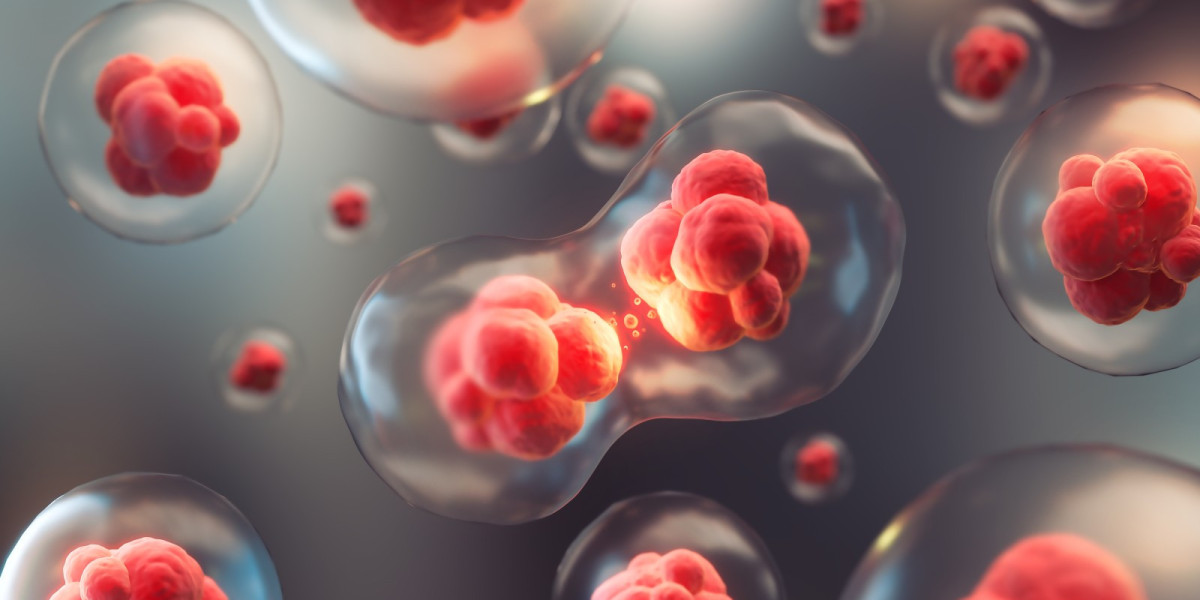
Mechanisms of Induced Pluripotency
The process of cellular reprogramming that generates iPS cells is highly complex, involving widespread epigenetic and transcriptional changes. The four transcription factors - OCT4, SOX2, KLF4, and c-MYC - work together to initiate a cascade of molecular events that gradually converts the epigenetic identity and gene expression profile of the adult cell towards that of an embryonic stem cell. Studies using global gene expression profiling have revealed that complete reprogramming occurs gradually through partially reprogrammed cellular intermediates. Exactly how these factors cooperate to orchestrate the erasure of the somatic epigenome and activation of the pluripotency network on a genome-wide scale is still not fully understood. Emerging evidence also suggests that epigenetic regulators and non-coding RNAs play important roles in reprogramming by facilitating chromatin remodeling and silencing of somatic genetic programs.
Advances in Reprogramming Methods
Considerable effort has gone into developing improved methods for generating clinically applicable Global Induced Pluripotent Stem Cells. Early reprogramming methods relied on integrative viral vectors like retroviruses and lentiviruses to deliver reprogramming factors, which risked insertional mutagenesis. Current non-integrative approaches utilize sendai virus, plasmid vectors, synthetic mRNAs or proteins to reprogram cells without permanently altering their genome. CRISPR/Cas9 technology has also enabled the generation of integration-free iPS cell lines through precisely editing out reprogramming factor cassettes after reprogramming is complete. Other refinements include defined chemical cocktails that induce pluripotency more efficiently and stoichiometrically controlled reprogramming using synthetic transcription factors. These advancements have made iPS cell technology safer and better equipped for therapeutic applications.
Modeling Disease Using Patient-Specific iPS Cells
A major application of iPS cell technology is in the modeling of human diseases. Patient-specific iPS cells can be directly reprogrammed from readily accessible tissues like skin biopsies. When grown in culture and differentiated into various cell types, these disease-specific iPS cell lines recapitulate disease-relevant phenotypes. For instance, iPS cell-derived neurons, heart or pancreatic beta cells from patients with neurological, cardiac or metabolic diseases respectively can provide invaluable cellular models for probing disease mechanisms and screening drugs. Such models have already offered new insights into complex diseases like Parkinson's, amyotrophic lateral sclerosis, diabetes and others difficult to study otherwise. With continued refinement, iPS cell-based disease modeling holds great promise to revolutionize our understanding of pathogenesis and accelerate the discovery of targeted therapies.
Advancing Clinical Translation of IPS Cells
While iPS cell technology was originally conceived as a potential unlimited source of patient-matched cells for transplantation therapy, bringing iPS cell-derived grafts to the patient bedside still faces major challenges. Chief among these are ensuring complete reprogramming, consistent differentiation into mature functional cell types, and the long-term safety of grafted cells post-transplantation. Considerable effort is ongoing to address these hurdles through genomic validation, optimized differentiation protocols using biomaterials and 3D organoids, and safety switches to eliminate transplanted cells if needed. Recent clinical trials have taken initial steps, implanting retinal pigment epithelium cells in patients with macular degeneration and using cardiomyocytes in heart disease. With continued progress, iPS cell transplantations may become a promising reality for treating conditions like Parkinson's disease, diabetes, spinal cord injuries and more within the coming decade.
Global Research Efforts and Regulatory Landscape
Research using human pluripotent stem cells is now a large, global enterprise encompassing both academic laboratories and biotechnology companies. While Asia, and particularly Japan and China, were initially at the forefront of induced pluripotent stem cells research, activity has expanded greatly in North America and Europe in recent years. Large teams backed by strategic government investments are actively working towards realizing the potential of iPS cells. For example, the Stem Cell Network (SCAN) in Canada supports multiple translational projects while Germany's PluriNet initiative fosters collaboration between clinicians and basic scientists. Regulatory frameworks are also being established worldwide to provide oversight for clinical research with human pluripotent cells. In the US, the FDA has provided important guidance on oversight pathways for initial safety studies. International organizations like the ISSCR work to harmonize standards and share best practices as the field moves steadily towards the clinic. With continued global research partnership and prudent regulation, iPS cell based therapies may one day transform patient care.
Get more insights on Global Induced Pluripotent Stem Cells
![North America Electric Vehicle Market Size, Share & Trends [Report] 2030](https://biiut.com/upload/photos/2024/03/BUtkFdHBtC2VQQa2OJYZ_06_a4b8655688f67086b1bf9f32c1870eb4_image.jpg)

